
2.1 Case notifications
Tuberculosis (TB) case notifications refer to people diagnosed with TB disease and officially reported as a case to national authorities. Case notification data have been systematically collected at national level and then reported to WHO on an annual basis since the mid-1990s, based on standard case definitions and associated guidance on the recording and reporting of data provided by WHO. The most recent WHO guidance was published in 2024 (1).
Globally in 2023, 8.2 million people with a new episode of TB (referred to as new and relapse cases) were diagnosed and notified (Table 2.1.1). Of these, 84% had pulmonary TB and 16% had extrapulmonary TB. Collectively, the African, South-East Asia and Western Pacific regions accounted for almost 90% of total notifications, with close to half in the South-East Asia Region alone.
| WHO region | Total notified | New and relapsea | Pulmonary new and relapse number | Pulmonary new and relapse bacteriologically confirmed (%) | Extrapulmonary new and relapse (%) | People living with HIV, new and relapse | MDR/RR-TB onlyb | pre-XDR-TB or XDR-TBc |
|---|---|---|---|---|---|---|---|---|
| African Region | 1 917 797 | 1 882 966 | 1 654 538 | 69% | 12% | 314 460 | 21 482 | 1040 |
| Region of the Americas | 285 597 | 264 077 | 228 948 | 81% | 13% | 23 601 | 5819 | 309 |
| South-East Asia Region | 3 992 545 | 3 831 189 | 3 056 843 | 60% | 20% | 64 245 | 70 531 | 13 767 |
| European Region | 171 355 | 148 633 | 125 905 | 70% | 15% | 19 184 | 29 459 | 10 599 |
| Eastern Mediterranean Region | 645 236 | 638 521 | 494 080 | 55% | 23% | 2087 | 5150 | 1085 |
| Western Pacific Region | 1 418 659 | 1 394 737 | 1 293 773 | 58% | 7% | 13 228 | 27 243 | 2182 |
| Global | 8 431 189 | 8 160 123 | 6 854 087 | 62% | 16% | 436 805 | 159 684 | 28 982 |
b RR-TB, rifampicin-resistant TB; MDR-TB, multidrug-resistant TB (defined as TB that is resistant to rifampicin and isoniazid). This column excludes any cases with known resistance to any fluoroquinolone.
c XDR-TB, extensively drug-resistant TB. Pre-XDR-TB is defined as TB that is resistant to rifampicin and to any fluoroquinolone. XDR-TB is TB that is resistant to rifampicin and to any fluoroquinolone, and to at least one of bedaquiline or linezolid.
The 8.2 million people newly diagnosed and notified with TB in 2023 is the highest number for a single year since WHO started to compile data from all countries and areas in the mid-1990s, up from the previous record of 7.5 million in 2022 and 15% higher than the pre-pandemic level of 7.1 million in 2019 (Fig. 2.1.1). These two years of record levels of TB case notifications follow two years of COVID-related disruptions to health services, when TB case notifications fell considerably below pre-pandemic levels, most noticeably in 2020 (with a global reduction of 18%, to 5.8 million) before a partial recovery in 2021 (to 6.4 million).
The historically high numbers in 2022 and 2023 show that there has been a strong global recovery in the provision of and access to TB diagnosis and treatment. It is likely that they also reflect two other factors: the diagnosis of a backlog of people who developed TB in previous years but whose diagnosis was delayed by COVID-related disruptions, and an estimated increase in the overall number of people developing TB disease (Section 1.1).
Trends in case notifications in the six WHO regions before, during and in the aftermath of the COVID-19 pandemic vary (Fig. 2.1.2). The pattern in the South-East Asia Region is very similar to the global trend, with a big reduction (-24%) between 2019 and 2020 followed by a partial recovery in 2021 and then a strong rebound to above the pre-COVID level in 2022–2023; indeed, it is this region that drove the trend at global level. There were similar patterns in the Eastern Mediterranean Region (mostly influenced by trends in Pakistan) and the Region of the Americas.
In the European Region, notifications fell at a rate above the historic trend in 2020, increased in 2021 (likely representing some backlog from 2020) and then returned to a downward trend in 2022–2023. In the Western Pacific Region, case notifications in 2023 recovered to the 2019 level, following a big drop in 2020–2021. The recovery in 2023 in the Western Pacific Region was driven by China and the Philippines, which together accounted for 81% of total notifications in the region in the five years 2019–2023 (Fig. 2.1.3).
It is striking that notifications in the African Region increased throughout the pandemic and that this has continued in its aftermath. In 2023, the reported number of people newly diagnosed with TB was 34% above the level of 2019.
By 2023, case notifications in most of the 30 high TB burden and three global TB watchlist countries had recovered to the pre-COVID level or beyond (Fig. 2.1.3). The exceptions were Angola, Lesotho, Liberia, Mongolia, Myanmar, Thailand and Zimbabwe. Two countries reported declines during and after the COVID-19 pandemic that were consistent with historic trends: the Democratic Republic of Korea and the Russian Federation.
Most notified cases of TB are among adults (Fig. 2.1.4). Of the global total of people notified as a new or relapse TB case in 2023, 56% were men, 35% were women and 8.5% were children aged 0–14 years (the age groups related to children for which WHO routinely collects data are 0–4 and 5–14 years; it is recognized that the second category includes young adolescents). For the remainder, either age or sex were unknown. In general, notification data appear to understate the share of the total TB disease burden that is accounted for by men, since higher male to female ratios among adults have been found in national TB prevalence surveys (Section 1.4). The drop in case notifications between 2019 and 2020 and subsequent recovery was similar for men and women, while both the drop in 2020 and subsequent recovery were more pronounced for children.
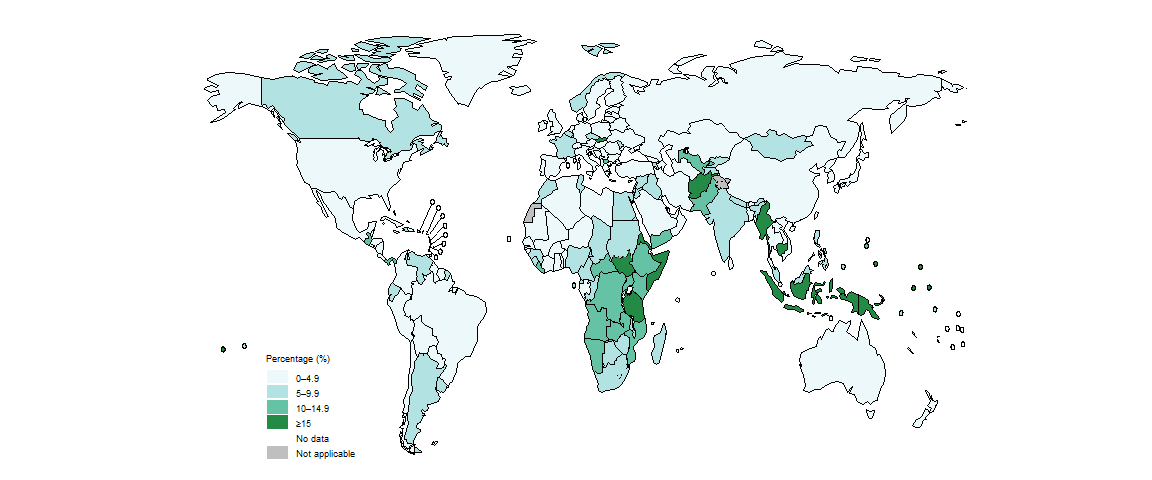
Although the global proportion of notified cases accounted for by children aged 0–14 years has been relatively stable (Fig. 2.1.4), there is considerable variation at country level (Fig. 2.1.5). Among the 30 high burden countries, those with particularly low levels (<5%) included Bangladesh, Brazil, China, Gabon, the Democratic People’s Republic of Korea, Thailand and Viet Nam.
There are recognized issues with the diagnosis and reporting of TB in children, including the use of variable case definitions and underreporting of cases diagnosed by paediatricians in the public and private sectors. Greater attention to the quality of TB notification data for children is warranted in many countries.
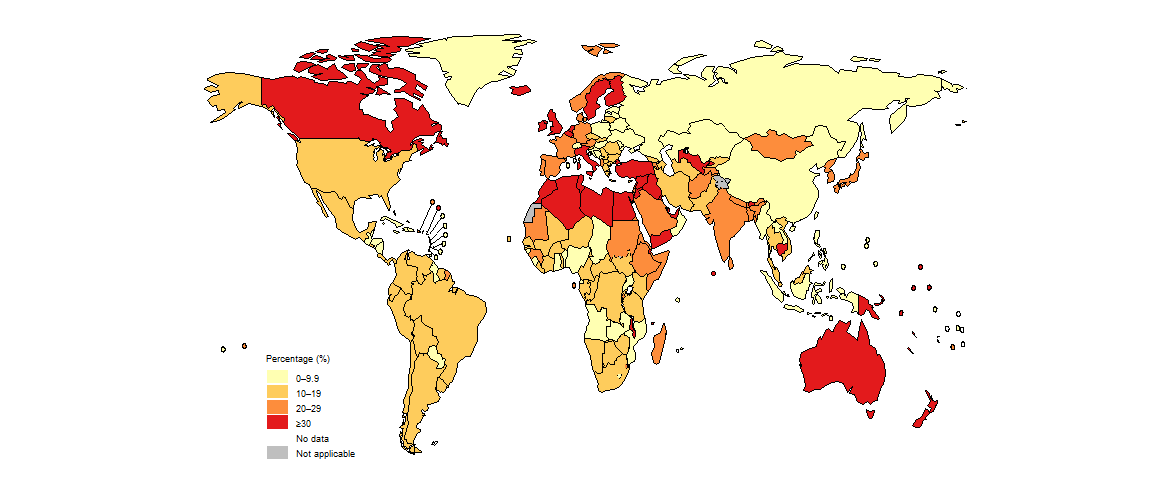
There is also considerable country variation in the proportion of notified cases diagnosed with extrapulmonary TB (Fig. 2.1.6). This may reflect underlying differences in TB epidemiology as well as diagnostic practices.
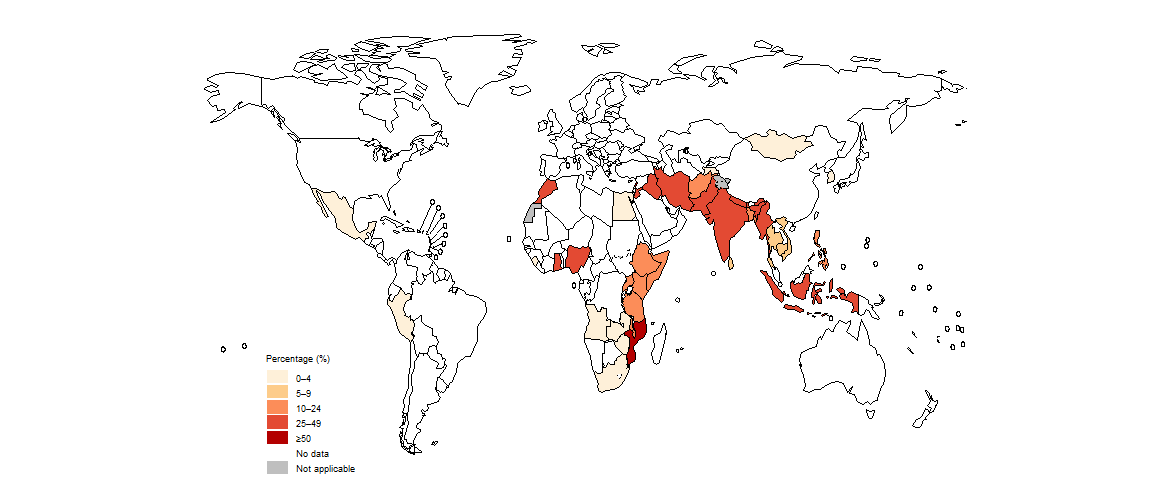
There is striking country variation in the distribution of TB case notifications according to country of origin (Fig. 2.1.7). In several countries with a low incidence of TB, more than 75% of notified cases were among people of foreign origin.

People housed in prisons or congregate settings have a high risk of developing TB and of having poorer TB treatment outcomes than the general population. Prisons can exacerbate ill health: for example, if there is chronic lack of investment in the justice sector, contraventions of human rights, low prioritization of health and harm reduction services in prisons, and an absence of other justice-based alternatives to incarceration. The physical infrastructure of prisons, including the risk of overcrowding and the frequent movement of prisoners can all increase the risk of transmitting airborne diseases such as TB.
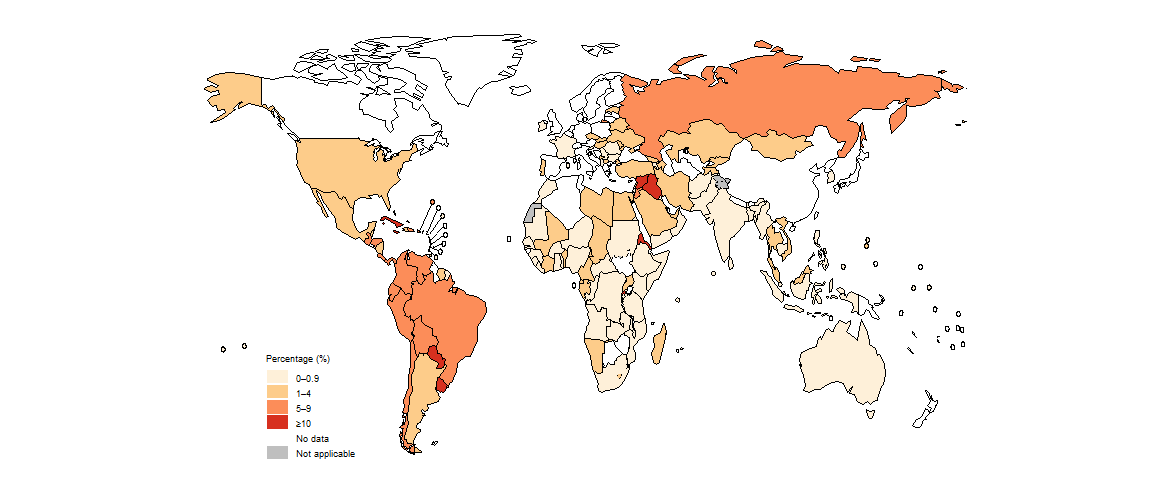
Data about the number of people notified as a new and relapse case of TB who were registered in prisons have been collected from all countries in the European Region since 2014 and from all countries in the Region of the Americas since 2018. Data collection was expanded to all countries in 2023; 144 countries and areas reported data. These data reveal considerable country variation in the percentage of people notified as a new and relapse case of TB who were registered in prisons (Fig. 2.1.8). The highest percentages are in countries and areas in the Region of the Americas.
Engagement of all care providers in the public and private sectors through public–private mix (PPM) initiatives can help to minimize the underreporting of people diagnosed with TB. Since 2015, the contribution of such PPM initiatives to total notifications has grown in most of the seven countries defined as top global priorities for PPM (Fig. 2.1.9).
b Public-public mix refers to engagement by the NTP with public health sector providers of TB care that are not under the direct purview of the NTP. Examples include public hospitals, public medical colleges, prisons and detention centres, military facilities and public health insurance organizations.
There is considerable country variation in the percentage of people notified as a TB case by public-private mix initiatives (Fig. 2.1.10).
b In 2023, WHO requested 42 countries to report data about the number of people notified as a TB case through public-private mix initiatives, of which 38 countries reported data.
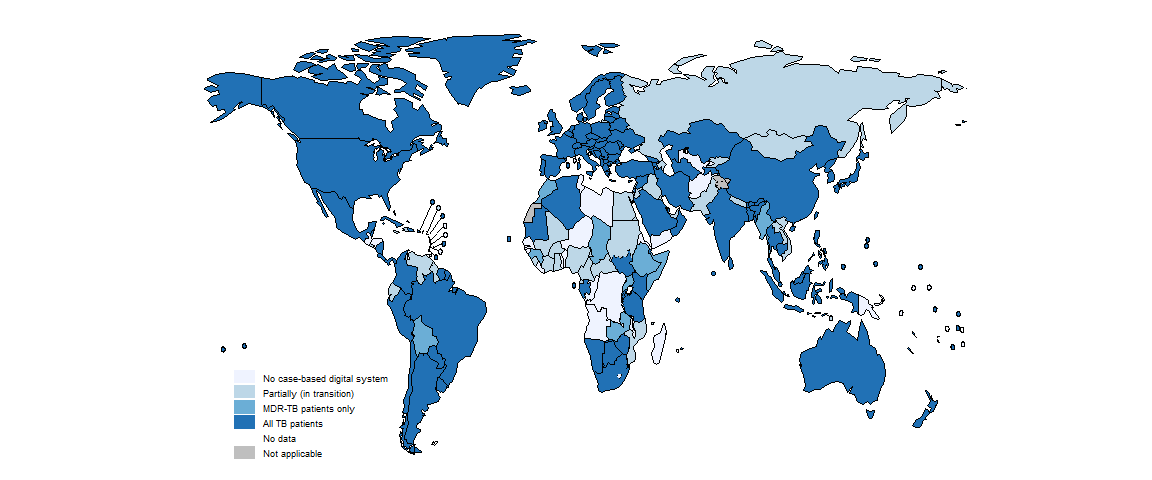
Case-based digital surveillance systems enable timely reporting and use of TB data; their main advantages are highlighted in the latest WHO guidance on TB surveillance (1). In 2023, 133 countries and areas that collectively accounted for 70% of officially notified TB cases were using a case-based digital surveillance system that covered all people diagnosed with TB (Fig. 2.1.11). This was similar to the level of 2022, when 132 countries and areas that collectively accounted for 65% of officially notified TB cases were using such systems. Acceleration of progress in making the transition from paper-based reporting of aggregated TB data to case-based digital TB surveillance is particularly needed in the African Region.
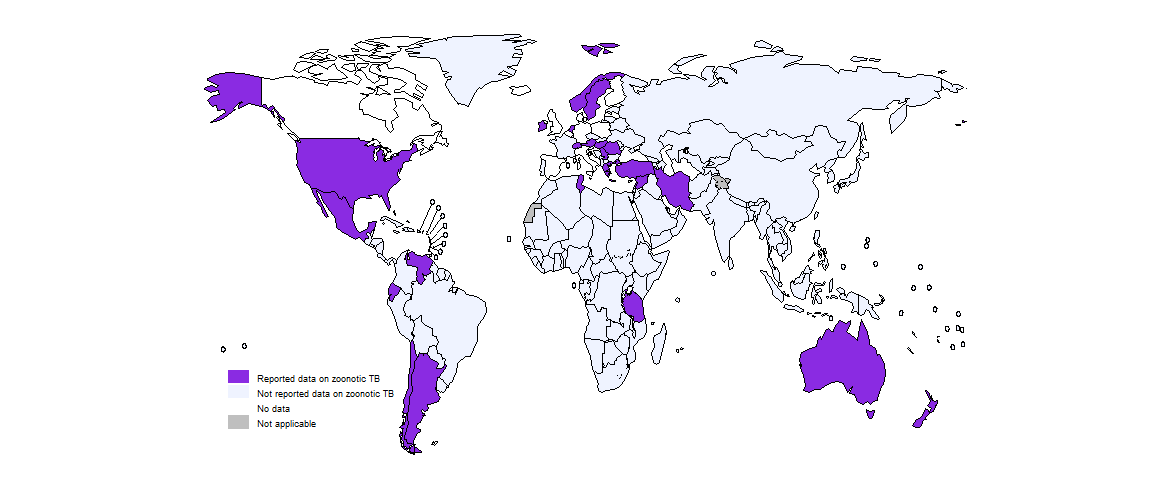
Zoonotic TB is a form of TB in people caused by a subspecies of the M. tuberculosis complex that is usually found in animals, such as M. bovis, M. orygis, M. caprae or M. pinnipedii. In 2023, 26 countries reported cases of zoonotic TB to WHO; the total number of cases was 371 (Fig. 2.1.12). This low number suggests that detection of zoonotic TB remains sub-optimal.
Data shown on this webpage are as of 29 July 2024 (see Annex 2 of the core report document for more details).
References
- Consolidated guidance on tuberculosis data generation and use: module 1: tuberculosis surveillance. Geneva: World Health Organization; 2024 (https://iris.who.int/handle/10665/376612).
