Caption: Flyer of the 9th webinar of the series of second Annual Malaria Research in Indonesia. Various challenges of and perspectives on the malaria programme were discussed by national and international researchers. Photo credit: NMCP 2020
As Indonesia progresses on its path to achieve 75% of the country free of malaria by 2024, scientists and researchers gathered at the Annual Malaria Research in Indonesia (AMRI) Seminar to exchange insights on the future of malaria surveillance, diagnosis, and treatment in the country.
Held virtually through ten webinar sessions, the AMRI Seminar was organized by the National Malaria Programme (NMP) of the Ministry of Health (MoH) in collaboration with the Indonesian Association of Researchers on Parasitic Diseases (P4I) and Indonesian Public Health Entomologist Association (PEKI), WHO, and UNICEF.
The use of online-based applications and digital-based approaches in the malaria programme were some of the innovations brought forward in the AMRI seminar. The Province Health Office (PHO) of East Nusa Tenggara presented the use of an electronic and online malaria readiness self-assessment tool malaria elimination efforts. By using this tool, health workers could track the progress of malaria intervention activities from the primary health centre up to the province level, towards achieving a free malaria district.
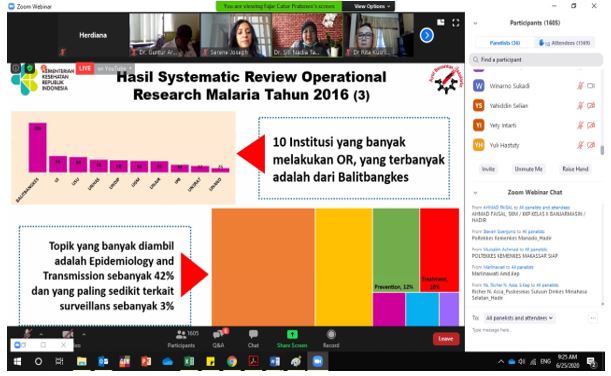
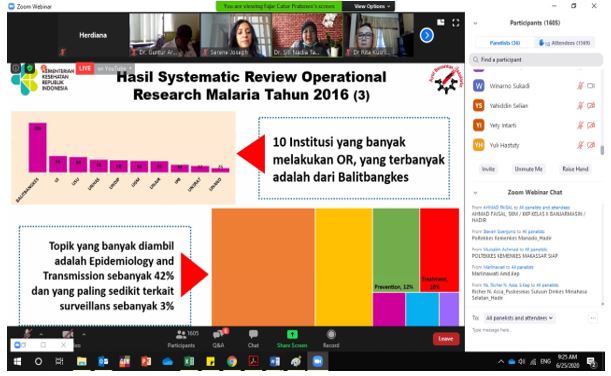
Caption: The Director of Vector Borne and Zoonotic Diseases Prevention and Control presented the findings from systematic review of malaria operational research in Indonesia conducted in 2016. Photo credit: WHO Indonesia 2020
Health officials from Fakfak District, West Papua Province, shared their innovative ‘defence and offence’ surveillance approach in the Bela Kaca programme (No Malaria, Brighter Village) programme. Under this programme, health workers will launch a comprehensive intervention or ‘offense’ for two months in villages where five or more malaria cases are present. When cases have dropped to zero, strict community-based surveillance will be implemented, and the community will devise the 1-2-5 strategy when a new case is found. This means that on day one, the case will be examined and notified to the higher level. An epidemiological investigation will be launched by day two to inform the epidemiological intervention on day five. This method has successfully brought down the number of malaria cases from 1743 cases in 2017 to 180 cases in 2019.
The importance of community perception on malaria was highlighted in research titled ‘Why should it be a priority to understand malaria in Tanah Papua?’ presented by dr Enny Kenangalem from the Health Development and Papuan People Foundation (YPKMP) Timika. On a similar topic, Mara Ipa from the National Institute of Health Research and Development (NIHRD), MoH reported her analysis from basic health survey 2018 on the heterogeneity of preventive practices and their relationship to malaria infection in Eastern Indonesia. The study found that adult men with low education level, and those who were unemployed were likely to report having malaria. The study also indicated that providing long-lasting insecticidal nets (LLINs) to protect the community against malaria transmission without appropriate educational messages did not significantly impact malaria case reduction.
Other interesting findings presented in the AMRI seminar included malaria intervention in the form of counselling individuals to prevent Plasmodium vivax malaria recurrence and research by I Made Winarta highlighting the high prevalence of malaria among army troops in northern Papua that require faster diagnosis, availability of malaria medicines, vector control and multi-disciplinary approaches.
Vector biology, vector control interventions and insecticide resistance were discussed in a panel joined by the MoH Malaysia (Kementerian Kesihatan Malaysia/KKM)
and the United States Centers for Disease Control and Prevention (US CDC). The researchers from Malaysia shared their research on outdoor residual spraying as vector control measure to reduce Plasmodium knowlesi cases. This research is relevant to Indonesia due to the concerns around outdoor malaria transmission and the paucity of research conducted in this area. Researchers from the Eijkman Institute, the Institute for Vector and Reservoir Control Research and Development (BBPPVRP) Salatiga, University of Lampung, University of Airlangga and regional technical health environmental and diseases control unit (B/BTKLPP) staff also presented their studies of malaria vector-related issues.
The Faculty of Medicine, Gadjah Mada University (UGM) presented an innovation called ‘digital-based microscopic cross-checking system’. Cross-checking is part of quality control to ensure the accuracy of malaria examination. It is a system whereby a sample of routine blood
slides are cross-checked for accuracy by a regional or national reference laboratory. Some laboratories face challenges in conducting physical cross-checking of microscopic results, including distance, time, and transportation cost for sending slides to the Provincial Health Office or other reference laboratories. UGM team has succeeded in developing a digital-based malaria microscopic cross-checking system to overcome these challenges. Using the digital-based approach, microscopists at the community health centre (puskesmas) are equipped with a digital device attached to a microscope to take microscopic images of malaria parasites and are trained to use the digital cross-checking system. Successful implementation of this method is expected to improve the accuracy of diagnosis at the sub-district level, contribute to external quality assurance and eventually support the government in the malaria elimination programme.
Malaria treatment issues in Indonesia discussed during the AMRI seminar were the new potential of artemisinin-based combination therapy (ACT) for second line treatment and a candidate of new ACT to replace the current drug used in the malaria programme, namely dihydroartemisinin piperaquine (DHA-PPQ), which has been used for more than 15 years and demonstrated an increasing trend of late treatment failure.
The last two webinars discussed the future of malaria in Indonesia to support malaria elimination by 2030. There was productive discussion between WHO, international researchers from Menzies School of Health Research, Australia and the University of Notre Dame, US, and national researchers on the challenges of achieving malaria elimination in Indonesia. Among the key challenges are the high burden of hidden parasites in the liver for P. vivax, mobile and migrant populations, and outdoor transmission interventions.
After seven years of applying subnational certification of malaria elimination from the district level, the National Malaria Control Programme (NMCP) and representatives of Central Kalimantan and Jambi provinces shared their lessons learnt and challenges to support the districts in achieving successful malaria-free certification process and ensuring required data and documentation as evidence that there has been no local transmission in the district in the last three consecutive years.
This final session of AMRI seminar was officially closed by the MoH Director of Direct Infectious Diseases dr Siti Nadia Tarmizi with a note to encourage sustaining the excellent collaboration among malaria programme with research communities and professional organization in evidence-based policy making.